What if we viewed lived experience as an asset? As an asset of professional, economic,…

Personalised Care & Palliative Care: How Can They Help Each Other?
I’ve been writing this blog for a few weeks now but got interrupted by my admission to hospital with sepsis last Sunday. Then yesterday I saw a blog by Tracey Bleakley, CEO of Hospice UK, talking about the very subject of this blog – great minds think alike? At least I hope so. As a result, I will quote Tracey through this blog now I have her fantastic article to take inspiration from as I edit, cut back and finalise my blog into its final form from the rambling free-flowing text that this is presently, at the time of writing this introduction.
As a palliative care patient of over seven years, I know the true benefit of palliative care. Palliative care has not only looked at my illness, but at my life, quality of life and experiences, seen me as a unique individual and view me as a whole person, not a sum of parts made up of various medical specialities. They see the ‘big picture’, not just my internal bodily systems but both my internal and external life, including my support network, my social needs and my wishes, goals and aspirations for my life. They have managed my symptoms to maximum efficacy, facilitated my desired quality of life, empowered me to chase my dreams and goals and supported my family. However, it goes deeper than that. I truly believe palliative care is the reason I have exceeded my prognosis, it is the reason I am still here, and research does show that palliative care can actually extend life. It may seem strange to some, but the last seven and a half years that I’ve known my condition was going to drastically shorten my lifespan, have been the best years of my life in some respects; and palliative care is the reason for that. I have been able to carve a life for myself both because as well as in spite of my illness, a life that is fulfilling, enjoyable and productive. I have been able to contribute to society, make a difference, put my stamp on the world, and to create my legacy. I have been able to make constructive use of my experiences and suffering, to benefit others. I have been able to be a voice for others and to be a conduit to enable their stories and experiences to be heard and recognised. Over the last seven and a half years, I’ve lived life to the full, achieved a great deal and had an amazing time, despite the presence of my illness and the difficulties, struggles, suffering, complications, treatments, admissions, difficult conversations and harsh realisations it has resulted in.
However, I only receive this palliative care because I have a diagnosed life-limiting condition. I am supported by a hospice, a palliative care consultant, on the local end of life register, have an advance care plan in place and a care package in my home that supports me to survive and thrive now, but will also enable choice and control over where I am at end of life, as I have specialist care within my home. What about all the other people with long-term, but not life-limiting conditions who could also benefit from the care and support I receive from palliative care? They could benefit from the holistic, person-centred, personalised care that palliative care provides, they could benefit from an emphasis on symptom control, they could benefit from the psychosocial, emotional, spiritual and wellbeing support, they could benefit from having professionals in their lives who focus on care and not just on scrabbling for a cure and feeling lost when one is not available. Why shouldn’t they have access to this care, too?
Then comes reality. Hospice and palliative care services cannot keep up with demand for their services as it is for individuals with life-limiting conditions, with over 200,000 needing and qualifying for the support of hospices, let alone then supporting the 15 million people with one or more long term condition in the UK. It is not sustainable, especially when you consider most hospices are charities and derive most of their funding from donations, fundraising, grants and corporate and other support. However, could the NHS and social and other services provide this palliative approach within existing services? I am in two minds about whether this can be fully achieved to the same degree and success as palliative care has achieved for many years. This integrated approach to care requires a huge culture shift and an openness to a new way of working, as well as all the services being integrated and collaborating and the patients themselves having their care built around them from the first point of contact to end of life. Is there currently the infrastructure for the NHS and social care and allied services to provide a palliative, integrated and holistic, joined-up approach to care in the same way and to the same degree as the hospice and palliative care sector?
There is something happening in the NHS and social care today that will lead to a more palliative approach in some respects: personalised care. What is personalised care? According to NHS England, personalised care is as follows:
“Personalised care…takes a whole-system approach, integrating services including health, social care, public health and wider services around the person. It provides an all-age approach from maternity and childhood through to end of life, encompassing both mental and physical health and recognises the role and voice of carers. It recognises the contribution of communities and the voluntary and community sector to support people and build resilience.”
It also means:
“…people have choice and control over the way their care is planned and delivered. It is based on ‘what matters’ to them and their individual strengths and needs. This happens within a system that makes the most of the expertise, capacity and potential of people, families and communities in delivering better outcomes and experiences. Personalised care represents a new relationship between people, professionals and the health and care system. It provides a positive shift in power and decision making that enables people to have a voice, to be heard and be connected to each other and their communities.”
Personalised care largely shares the same underlying principles as palliative care, showing the two are very closely aligned. As Tracey Bleakley reflects in her article on ehospice “…the World Health Organisation defines palliative care as ‘an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness’, which is ‘applicable early in the course of an illness’. Palliative care is centred on the person and not the condition/s or symptoms. It balances medical, social, spiritual and practical needs according to the priorities of the person, their family and their community. In this way, it is rooted in the same values as personalised care.”
This shows how closely palliative care and personalised care are aligned.
However, I think it goes deeper than just personalised and palliative care being closely aligned. I truly believe the palliative care movement and hospice and palliative care professionals should be supporting the personalised care agenda and the implementation of personalised care since they have used this model of care for many years via the modern hospice movement. I believe palliative care professionals could be drivers in training and facilitating personalised care across the health and social care service spectrum, imparting their wisdom and years of experience on how to successfully implement this methodology of care. Why doesn’t the NHS make use of the decades of experience, learning, wisdom, successes and failures and so on of the palliative care movement to enable them to successfully implement the personalised and palliative-like approach? I feel this is definitely something to consider.
So many patients with long-term conditions suffer to the same degree, sometimes more, than patients with life-limiting conditions and palliative care needs. They could benefit from this holistic, joined-up, integrated approach to care in the same way as people like me do, but they do not meet the criteria for palliative care. Also, as previously stated, the hospice and palliative care sector can barely support the more than 200,000 patients needing and qualifying for palliative care, let alone supporting the 15 million people with one or more long-term conditions. This is why personalised care is so vital, as it is making strides to provide this holistic, integrated approach to care for individuals with long-term but not currently life-limiting conditions. Their symptom burden can be just as great and they also suffer functional loss and a reduced quality of life, and could greatly benefit from care being built around their needs, their symptoms managed effectively and the services joining together to support them, as well as the capacity building for them and their families and support networks, to empower them to self-manage as much as possible. Not only will this benefit the patients and their families/carers, it benefits the health service as we attend primary care less and reduces our use of emergency services and A&E attendances.
My care is far from perfect, but palliative care has given me so much. It has managed my symptoms and given me a far superior quality of life to what I would have without it. I also believe it has extended my life and is the reason I have exceeded my prognosis by at least 2 years. It has also drastically reduced my dependence on GP support and emergency care, as myself and my family have the skills, capacity and support to manage at home, but also, my Continuing Healthcare (CHC) package which includes 16 hours per day of intensive care nursing, means I have the support to manage things at home. Combining this with having the hospice for support and who are happy to help or advise – albeit not out of hours currently, a palliative care consultant who can help us manage symptoms at home, the community nurses for advice and the ability to telephone or email my specialist hospitals and the teams within them for advice and support, this means I have a system in place to keep me at home for as long as is possible and to prevent unnecessary admissions. I have a care plan built around my needs and an advance care plan in place so that the GP, out of hours teams, paramedics and A&E, via SystmOne, all know that my preferred place of care is at home and what my preferred priorities for care and my wishes are. I also have copies of my advance care plan documents at home.
I wanted to talk about personalised care and how this correlates with palliative care, especially in relation to two aspects. However I will start by explaining more about personalised care.
The comprehensive model of personalised care centres around this triangle. There are the whole-population “universal” approaches, then the “targeted” approaches aimed at people with long term conditions, and finally the “specialist” approaches for people with complex needs like me. I fall at the top of the triangle. This means I benefit from the personalised care approaches through the totality of the triangle. I’ve touched lightly on a few aspects of personalised care, and there are more I have not touched on. Through the universal whole-population approaches, I benefit from shared decision making, an approach in which patient and professional are on an equal footing and they share the decision, the patient is given sufficient information and their views are paramount and they are supported and empowered to actively support the decision-making process. Enabling choice is another universal approach, giving patients the opportunity to chose where, when and how they are treated (within reason) and who by, empowering them to have that say in their care and where and how it is conducted. Then there is social prescribing, which I am not going to touch on today, but more can be found out about this here. As part of the targeted methods, I benefit from personalised care and support planning, supported self-management and peer support. Then as part of the specialist aspects, I benefit from Integrated Personal Commissioning and personal or integrated budgets. The latter I will talk about in a minute.
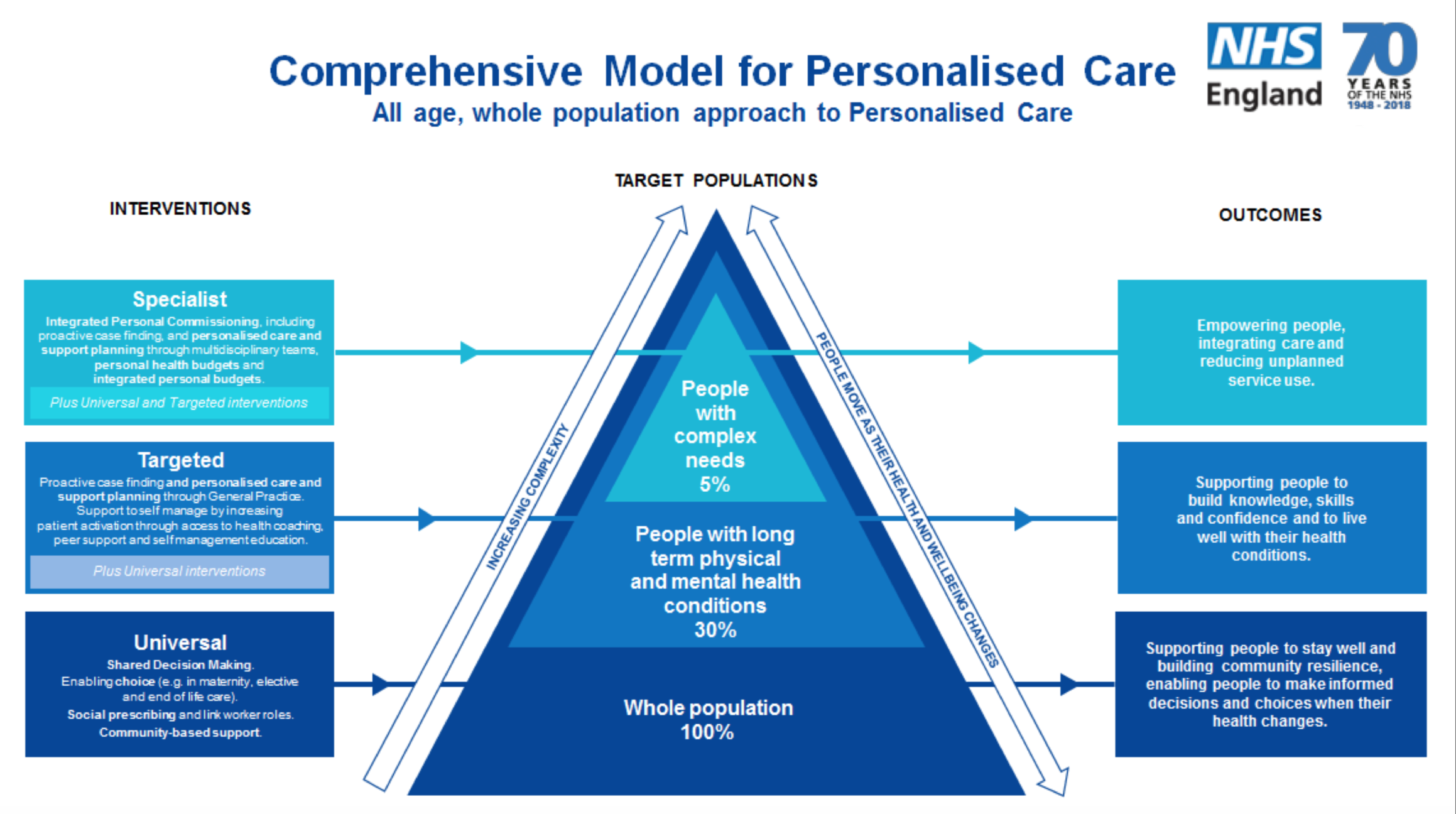
Image (c) NHS England
First, I wanted to touch on personalised care and support planning. This is a care plan which is created in partnership with the patient and with input from multiple professionals involved in their care, and is completely personalised to the patient, their needs, their wishes and desired outcomes. In my case, I actually have a few personalised care plans; my advance care plan being one of them, as well as my hospice care plan, and then my Continuing Healthcare (CHC) care and support plan. I have played a key role in the development of these care plans as well as who is involved in creating them. These care plans are built around the patient and the patient voice, needs and wishes are integral to the plan. It is about us, as patients, after all. This means we can have care built around and tailored to our personal needs, wishes and desired outcomes, based on a comprehensive, personalised care plan. From this plan, a tailored package and/or plan for the care of the individual can be built, and from this, shared decision making about what they would like and how their needs will be met, patient choice comes into plan to enable the patient to choose (within reason) the services and individuals involved in their care and how their needs are met, social prescribing may come into play and for those in the complex needs bracket, a personal or integrated budget may be created from this personalised care plan. Palliative care does this already: personalised plans are the centre of the patients’ care and then what services and support they receive is built around this plan. My first true experience of personalised care and support planning was with the hospice, and it was a liberating experience as it was my plan and the content of the plan was in my voice. What I wanted was put in there, and not what someone else dictated should be in there. I was able to have control over its contents and also how that information was conveyed, to ensure the plan was all about me and in my own words and my own voice. My palliative care nurse went away and wrote up the plan, then sent it back to me for me to amend – she was clear I needed to be happy with the plan and not just its content, but the wording, how it was laid out and phrases used, to ensure it was in keeping with me, my thoughts, my needs, my wishes and my voice.
Finally, I wanted to end with talking about Integrated Personal Commissioning (IPC) and personal budgets, and their link with palliative care. This is a reverse to my previous slant on this post, where I have been talking about palliative care’s impact on personalised care, now I will talk about a potential benefit of personalised care on palliative care. IPC is an approach that joins up the funding of health and social care and incorporating all available services, including the voluntary and community sector. This is to effectively commission services that meet the person’s needs holistically, integrating all available services into that individual’s package of care. I benefitted from IPC about five years ago when I became joint funded between the NHS and social care into an integrated budget, part of which I used to fund care from The J’s Hospice, my local young adult hospice-at-home service. Then, in 2014, I became fully health funded and went onto a Personal Health Budget (PHB). PHBs originated in a pilot that enabled individuals with NHS Continuing Healthcare funding to receive this in methods other than directly commissioned, block-contract type services. It enabled individuals to manage their CHC funding in the same way as social care funding can be managed, including via direct payments managed solely by the individual or with a third party supporting with the management of the financial aspect of the package. Sadly, my PHB fell apart when mum became unwell and I went onto a directly commissioned, agency provided CHC package as an interim measure. However, on 1st October phase 1 of my new Personal Health Budget went ahead, meaning my overnight care and double-up care is now managed via a PHB, and in the New Year we will begin to make strides with phase 2, which is transitioning the nursing aspect of my package onto my Personal Health Budget, meaning I will be 100% on a PHB and employing all my own staff. I cannot wait. This facilitates my desired quality of life best and gives me choice, control and autonomy over my life and care. It also means I can commission my own support services from my Personal Health Budget, as agreed in my care and support plan and with approval from the CCG.
I am a big believer that some of the answers to the funding deficiency in the hospice and palliative care sector, are Personal Health Budgets (PHBs), Integrated Budgets (IBs) and social care Personal Budgets (PBs). I have previously been able to fund some care from The J’s Hospice in my personal budgets, at a time when my Clinical Commissioning Group refused to fund The J’s in traditional contracts. Despite having been supported by The J’s Hospice since April 2011, it’s only in the last 12 months that my CCG have directly commissioned services from The J’s. For the years I was able to fund The J’s via my own budget, this provided a funding solution, albeit only one person with one package. Children’s hospices seem better at embracing funding from Personal Health Budgets, Integrated Budgets and Personal Budgets than the adult hospice sector, and maybe that’s because the adult hospice sector has fewer patients with such budgets. However, should hospices be doing more to encourage such budgets for palliative patients from first contact with the hospice or palliative care service? If hospices could support CCGs and Local Authorities with the initiation and creation of Personal Health Budgets, Integrated Budgets and social care Personal Budgets, this would help CCGs and LAs but also enable hospices to have their support of the patient built into the personal budget itself. It would also help join up the care of the individual with the budget, by integrating health, social care and voluntary sector services, and since hospices do personalised care and support planning so well, they could ensure the care plan that is with the CCG and/or Local Authority was truly personalised, holistic and comprehensive and that it truly reflected the patient. However it could also have its services commissioned through the individuals’ budget, providing an additional funding stream for patient care.
I truly do believe that personalised care and palliative care are directly aligned, sharing the same underlying principles and the same desired outcomes: better lives, better care and joined-up support for patients with health needs. I believe palliative care could play a pivotal role in the roll-out of personalised care in the NHS and social care, sharing their learning from years of using a similar methodology to care for patients, and likewise the personalised commissioning and other aspects of personalised care could greatly benefit the hospice and palliative care sector.
Tracey Bleakley perfectly sums up how personalised care can benefit palliative care when she says:
“By adopting a wider personalised care approach, the 450,000 people who die each year who could benefit from palliative care could receive tailored help and support over a much longer period, and the 25% rise in demand expected by 2040 could be managed.”
I often use a quote in my speeches about palliative care, which also applies to personalised care:
“You can’t change the end result but you can improve the journey.”
By adopting personalised care throughout the NHS and social care, we can provide a more palliative, holistic and person-centred approach to care for all individuals, especially those with long term conditions, and palliative care can continue to provide support to individuals with life-limiting conditions, but also, with the joining up of the personalised care agenda with palliative care, we can ensure patients receive palliative care earlier and over a longer period to help them manage their conditions as they approach end of life, move through end of life and to their death, and then the support be in place for their families.
Personalised care and palliative care are two approaches to care that share the same DNA, the same heart. Let’s ensure they are closely aligned and both coexist and collaborate to ensure integrated, joined-up care for all.



This Post Has 0 Comments