What if we viewed lived experience as an asset? As an asset of professional, economic,…

NHS Peer Leadership Academy: Day 6 – The Final Day
And so it is, the final day of the Autumn 2018 cohort of the NHS Peer Leadership Academy. This continues with my series in which you can read previous blogs sharing my PLA journey by clicking the hyperlinked text for each day: Day 1, Day 2, Day 3, Day 4 and Day 5.
What an experience it has been. So much learning, personal development and growth, minds opened, networking and I come away with drive, passion and more ‘fire in the belly’ to go on and make a difference and contribute as much as I can to personalised care and its implementation. It has been a truly uplifting and memorable time – though we’re all sad that it’s over. Not only has the Academy itself been fantastic and a real once-in-a-lifetime opportunity, the people on the course as well as the team who run it – Jo, Rita, Steph and Colin – really made the experience 100% better. I have loved being on this course and meeting such incredible people who have inspired, motivated, moved and supported me and vice versa, and our friendships made on this course will truly last a lifetime. To know the whole group won’t be together, in one room again is sad, but we will, without question, stay in touch, continue our new friendships, meet up and maybe even collaborate and work together. We did mention having to do PLA reunions in future – so you never know! To be with people who all shared the desire to make a difference, to contribute to the development and roll-out of personalised care in the NHS (and social care), and to make positive and constructive use of our experiences to benefit others was just wonderful, despite being an introvert who needs time alone and space to re-energise (my Myers-Briggs personality type, ISFJ, fits me to a T), I have certainly been energised, inspired and benefitted from the collective passion of all the members of the Academy.
Our final day started with a quick few minutes touching base before the first story took place. This person’s story showed the journey towards personalised care and how when you encounter health challenges and/or disability, that you can end up in destinations you don’t want to get off at and to remain in, but with the right support and with persistence, you can get to the right destination eventually. It also showed us the impact and emotions of being in a place you don’t want to be and how you often have to be the driver to start the ball rolling with changing and improving the situation.
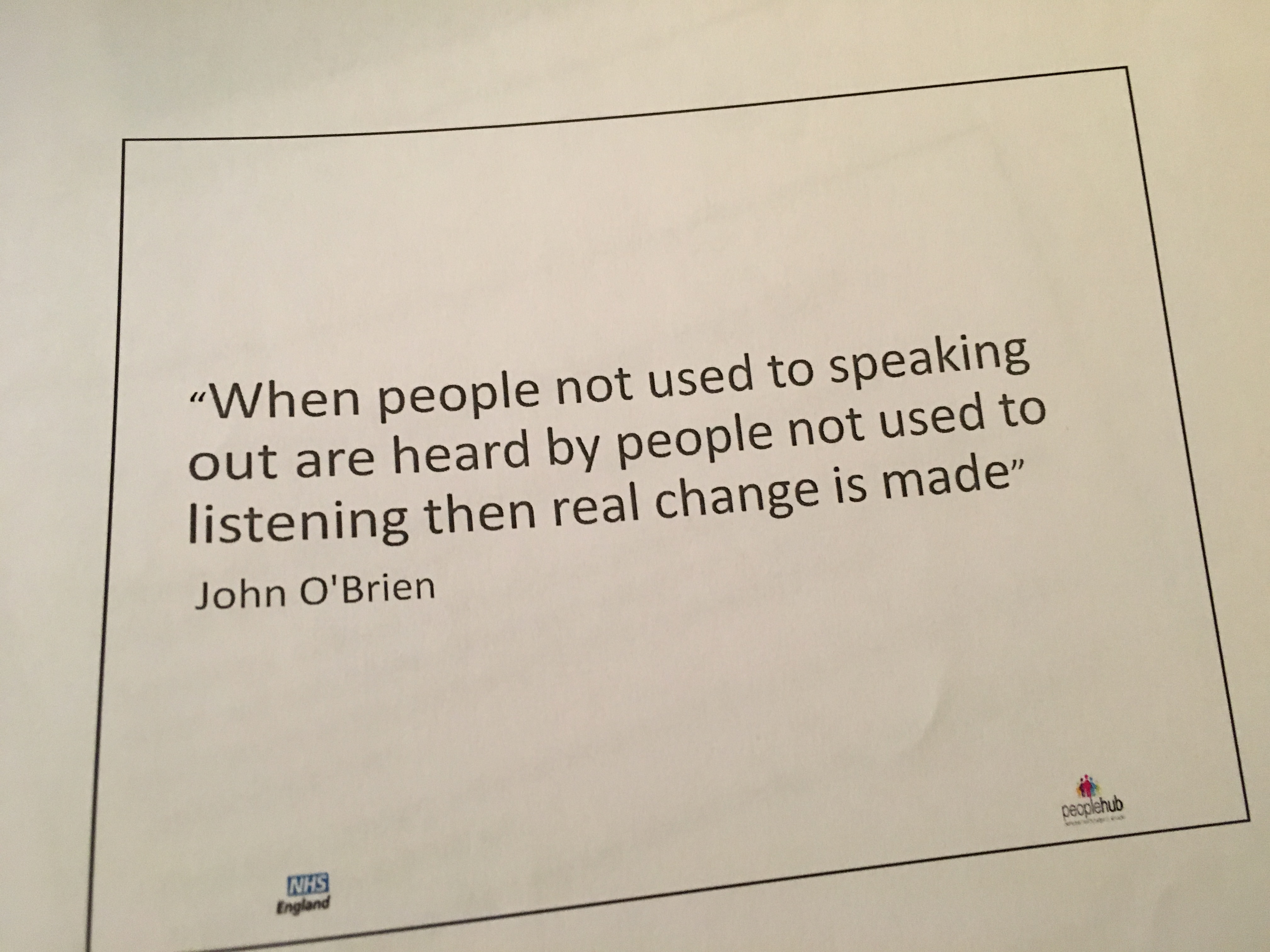
Today we were really challenged to think about the NHS professionals’ perspectives, difficulties and the culture that exists and to put ourselves in their shoes. Rita gave a thought-provoking presentation about organisational culture and how it can be overcome. We started off looking at the varying definitions of what culture actually is and the definitions that currently exist. We had to think about what culture is: it is the way organisations conduct their business, treat their employees, customers and the wider community; it is the extent to which freedom is allowed in decision-making and in developing new ideas and with personal expression; it is how power and information flows through their hierarchy; and how committed employees are towards collective objectives. Organisational culture is unique for each organisation and it is one of the hardest things to change. We looked at the barriers culture can create in the change management process, and there is an often used response from staff when change is being driven where people say “But that’s the way we’ve always done it!”, even with new staff who quickly absorb and participate in the culture of the workplace they work in and how they take on the values, beliefs and actions of the culture in which they work. We talked about culture in the NHS and healthcare more specifically and what structures matter most to culture change – the psychological and social structuring that govern how we think, what we value and what we see as legitimate. Rita shared how much of health system reform has tackled structural change, with less one about how people feel, think and behave as individuals and collectively. This can often be describes as the “software of the might” and can be thought of as its ‘culture’. Talk of an organisation’s culture is to assess what is shared by individuals within that organisation: their beliefs, values, attitudes and norms of behaviour. This may include routines, traditions, ceremonies and reward systems. Organisational culture encompasses the shared meanings that individuals place on their working life, the words and descriptions they use in making sense of their organisational context. The ways in which people understand, describe and make sense of their working context in turn help to define what is legitimate and acceptable in that context. They are “the way things are done around here”. We then thought of it as an iceberg: shared understandings may operate at different levels, and the most superficial are the visible manifestations – the things we see and recognise, like the tip of the iceberg that we can see above sea level. At a deeper level there are the values that are said to influence standard practice: a belief in evidence, for example, or a commitment to person-centred care. This is in the middle of the iceberg, the bit immediately below the surface. Then deeper still, the bottom of the iceberg, are much harder to access are the hidden assumptions that underpin day-to-day choices.
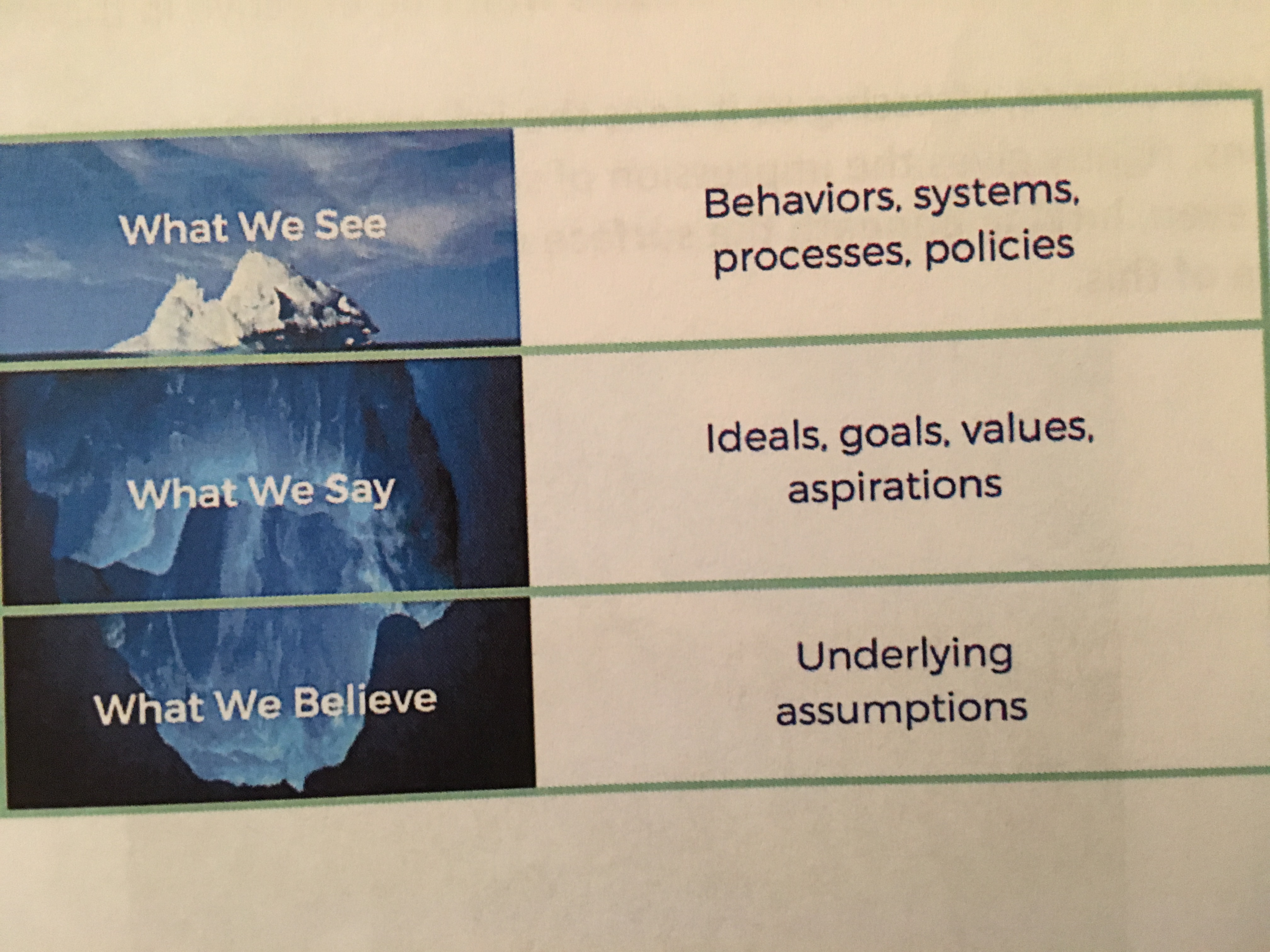
We then thought about how we might help influence that culture. We need to persevere and sustain ourselves for a lengthy process – change culture takes time and persistence. You may also encounter a lot of resistance. So what does this mean for us: we, as peer leaders, must think about culture and must understand it in order to make an impact. There is so much we don’t ‘see’ of an organisation, especially the informal unseen aspects of organisations, which gives the impression of something powerful, disruptive and even dangerous lurking beneath the surface of any organisation – this is something we must be aware of.
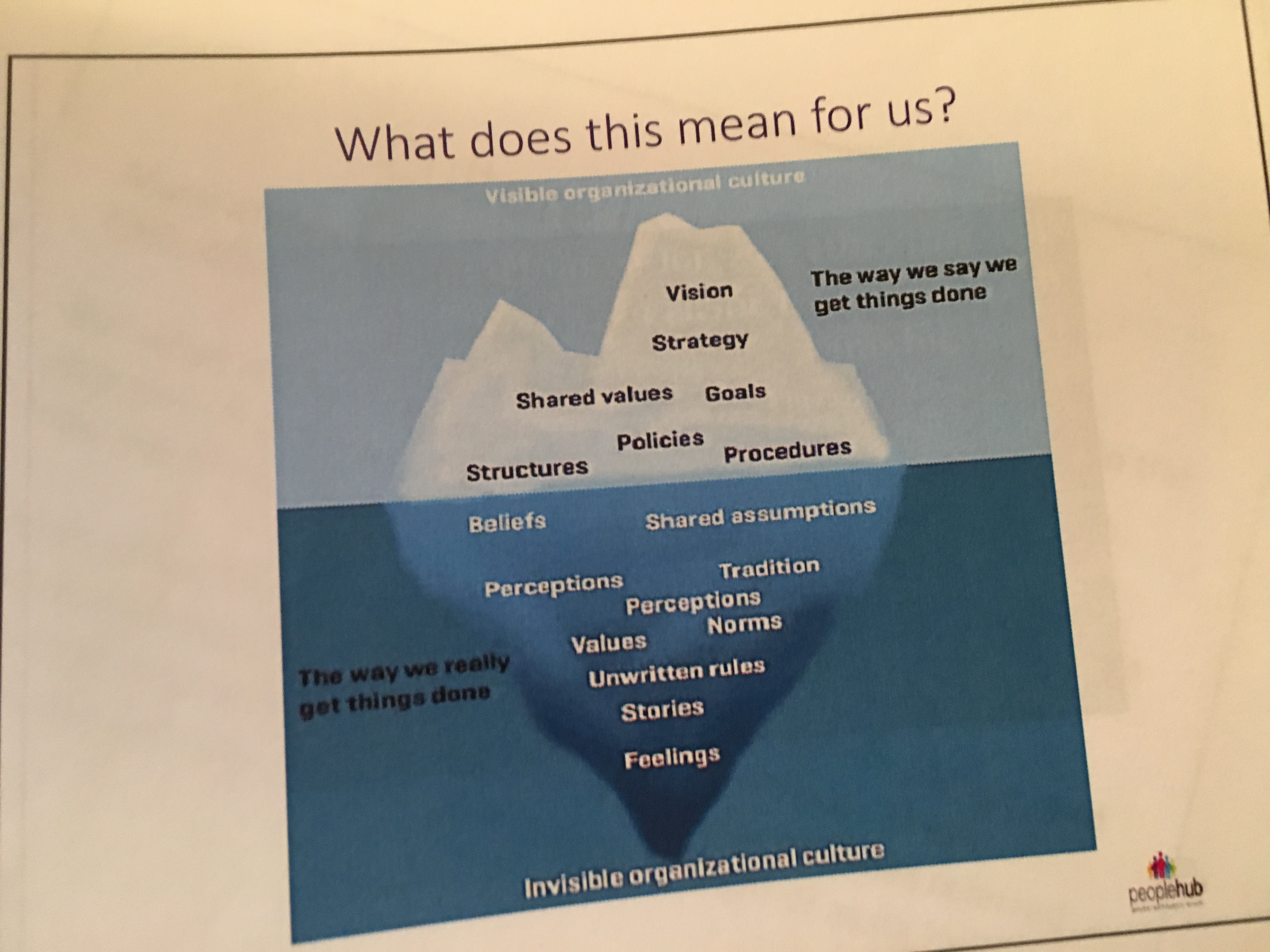
What have we learnt so far? Culture will not change simply by reconfiguring services or changing their location, because culture is about how we behave towards each other, what we say, think, value and assume. It’s about relationships with each other and with professionals and commissioners.
We then had to do an activity as if we were going to become a demonstrator sight and implement personalised care in our area. Our table decided to do this in the context of district nursing and we formulated a process of how we were going to implement it. We started off by saying we needed to understand the organisation, what works well and doesn’t, its culture and its ways of working in order to make changes. We would have to ‘sell’ personalised care to the various stakeholders, which we would do through a combination of workshops and open days, some with multiple stakeholder groups together but others specific to a certain stakeholder group, i.e. senior management, another for the front-line professions and another for patients. We would appoint champions within the organisation, staff members who could be the drivers and informers of the process and help make it a success, as well as having patient champions to ensure the patient voice was represented and to enable lived experience and patient perspectives to be input into the process. We thought about the various aspects, including selecting patient volunteers to be our “guinea pigs” (awful term) for the process who could be nominated by the professionals and be screened to ensure their experience would be beneficial and we had a representative sample, we needed to develop outcome measures on a strategic level, a feedback loop (which would be closed so patients had feedback on the process and what went well and didn’t) as well as before and after assessments of the patients involved looking at how well their outcomes within their personalised care and support plan had been met and the patients’ own reflections on the process and how they feel about how successful it has been, with clear measures such as improvements in quality of life, feeling more in control of their care and people feeling like their care is built around them. We then looked at a phased implementation of the different aspects of personalised care, with three phases and different aspects fitting into that, i.e. shared decision making would be from the outset, whereas Personal Health Budgets could fit into the various phases depending on need and demand, whereas social prescribing, we felt, would be rolled out in phase three. There would be constant rolling monitoring and evaluation to assess each stage of the roll-out, and to ensure that things are going well and changes to and improvements in how we are doing this can be made if not. We also recognised the financial aspect of this and thought about how and where funding would come from, but perhaps did not delve into this as much as we should’ve as, most importantly, where would the money come from? We then presented our plan to the whole room and all three tables had a lot of the same thoughts and focuses and Jo, Rita and Steph reflected on what they picked up from our plans and ideas and they were pleased that we’d really thought things through.
Then it was my story. Funnily, I was really nervous and this came across in my presentation, I don’t know why I got so nervous as I am used to presenting to hundreds of people at conferences, yet an intimate speech with my peers meant my nerves really got the better of me. I also could’ve improved my eye contact and relied less on my written speech – lots of great feedback from the group which is useful. I will put my speech and the slides at the bottom of this blog.
After lunch, another story was presented. A fantastic video made by the individual sharing their story and experiences and the impact that personalised care has had on their life. We both shared the knowledge that good personalised care had helped both of us to outlive our prognoses and both share the determination to continue defying the odds. It was moving and funny, informative and engaging, and really well done. I couldn’t think of any constructive feedback to give as it was so excellent.
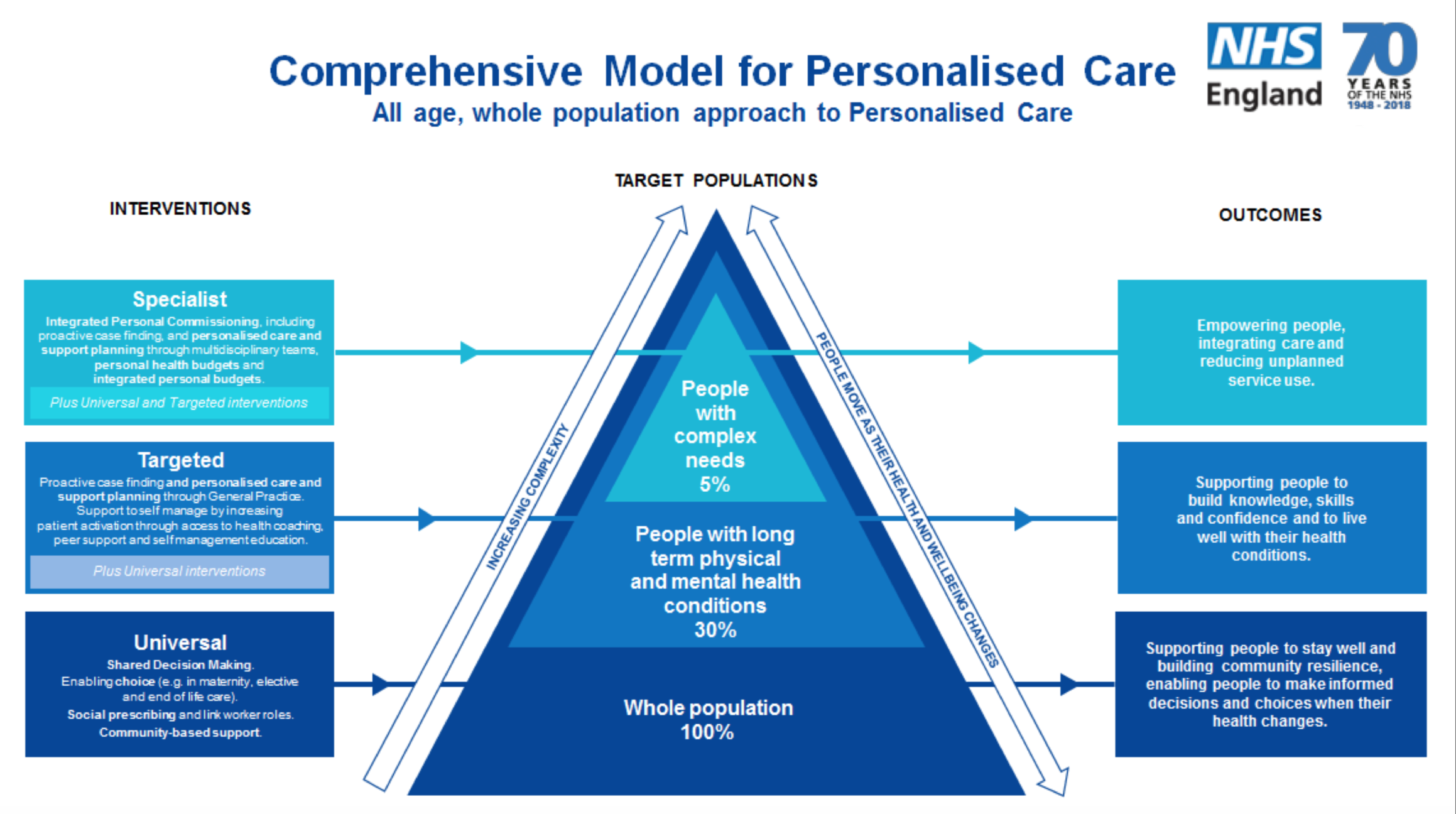
Next, James Sanderson, Director of Personalised Care at NHS England then spoke about what is happening in personalised care and what the future holds and how the development of the comprehensive model is really making and will continue to make a difference. We were then able to ask questions of James and some people asked some great questions and made some great points. One of the individuals asked about social prescribing and the barriers to GPs knowing what is available locally and how they can help their patients access it, which got it got me thinking – with the digital ambitions of the NHS, could we not develop a system in which GPs have a searchable database of all available local services so they can simply go onto their computer, search key words and it bring up various services in the area that may benefit their patient and the contact details to refer them on? Just a thought.
We then had the final story presentation which was fantastic, showing the journey she had taken through her life and spending time in a rehabilitation place and then a residential care home, before gaining a council bungalow and a care package, which was initially managed and provided by an agency and this worked for her, but as her mental and physical health improved, she wanted to take control over the package, and so she fought for a social care personal budget. She then shared her journey in meeting her now-partner, moving in together and getting married and how they both managed to secure Continuing Healthcare funding which they both manage via a Personal Health Budget, and the impact this has had and the responsibilities they have in managing their PHBs. It was a fantastic speech.
After a break, we then celebrated what we had learnt throughout the Peer Leadership Academy. We used vWall to share via digital post-it notes different things we’ve learnt in relation to different aspects of the programme and reading it was fascinating.
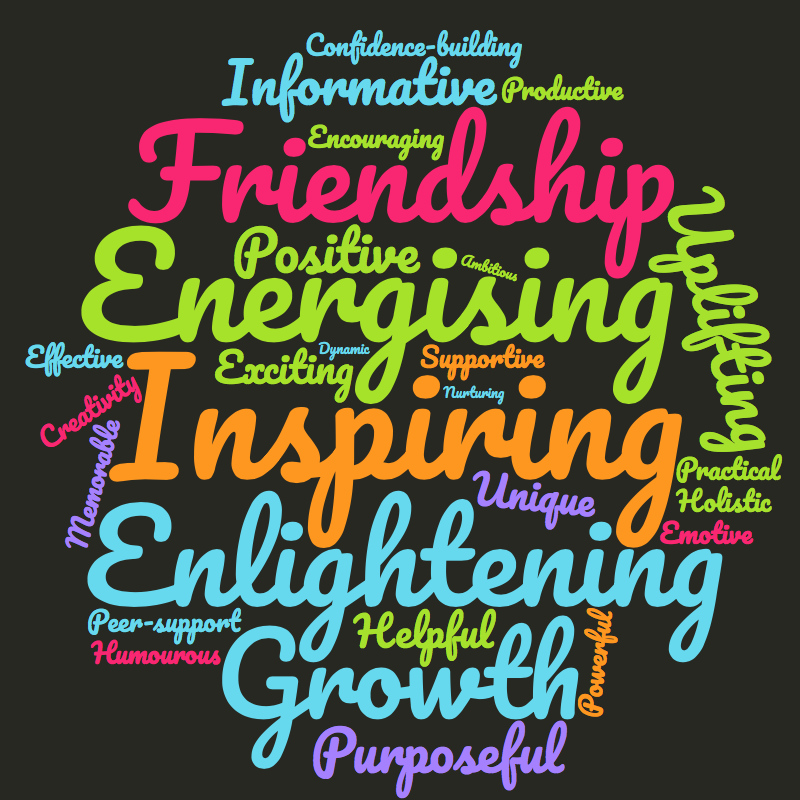
We were asked at the end to pick one word to describe our experience or takeaway from the PLA and gosh so many words rushed through my mind, picking one would be hard, so I said “motivated” but now, on my blog I thought I’d share a word cloud of some of the words that summed up my experience (although some of them I have used in this blog at various points anyway).
As I said, we’re all sad it’s over. It’s been an incredible experience and we are so grateful to Jo, Rita, Steph and Colin and other colleagues for making it happen. We have all learnt so much and made friendships for life, and I look forward to seeing how we all apply what we’ve learnt and what we do now and how we contribute to the personalised care implementation now and in the future.
Are you interested in participating in a future Peer Leadership Academy? Do apply when the applications open sometime early next year. Keep an eye out and I will be sharing it on my social media once applications open.
As promised, here are my speech and slides.

#HelloMyNameIs Lucy, as you all know, and I wanted to share some of my experiences in the context of personalised care and the impact this has had on my life.

I have complex medical needs as a result of my life-limiting condition, a condition I was born with but which did not cause too many restrictions until I became disabled and seriously ill at 14, despite having treatment and difficulties and my condition deteriorating throughout my childhood. It affects most organs and body systems and because it is progressive, it gets worse over time. It means I am dependent on intravenous nutrition, called TPN, through a central line into my heart, which is slowly pumped in over 21 hours a day. It is best understood when I say that TPN is the nutritional equivalent of life support, it gives you all your nutrition into your bloodstream because your digestive system cannot do its job, even with support, thus it has to be completely bypassed. This has kept me alive for over 7 years. In addition to TPN I have intravenous medications and fluids through my line every day. I also have a gastrostomy tube or PEG draining my stomach and two stoma bags, an Ileostomy which bypasses my colon and a Urostomy which has redesigned my urinary system. My condition means I need round the clock care and 16 hours of this is provided by an intensive care nurse, albeit my mum is trained to perform this care and does so when needed. At 17 I found out my condition was going to shorten my lifespan; at 18, I was told I wouldn’t survive another 5 years. I am proud to say I have currently survived at least 2 years beyond my prognosis.
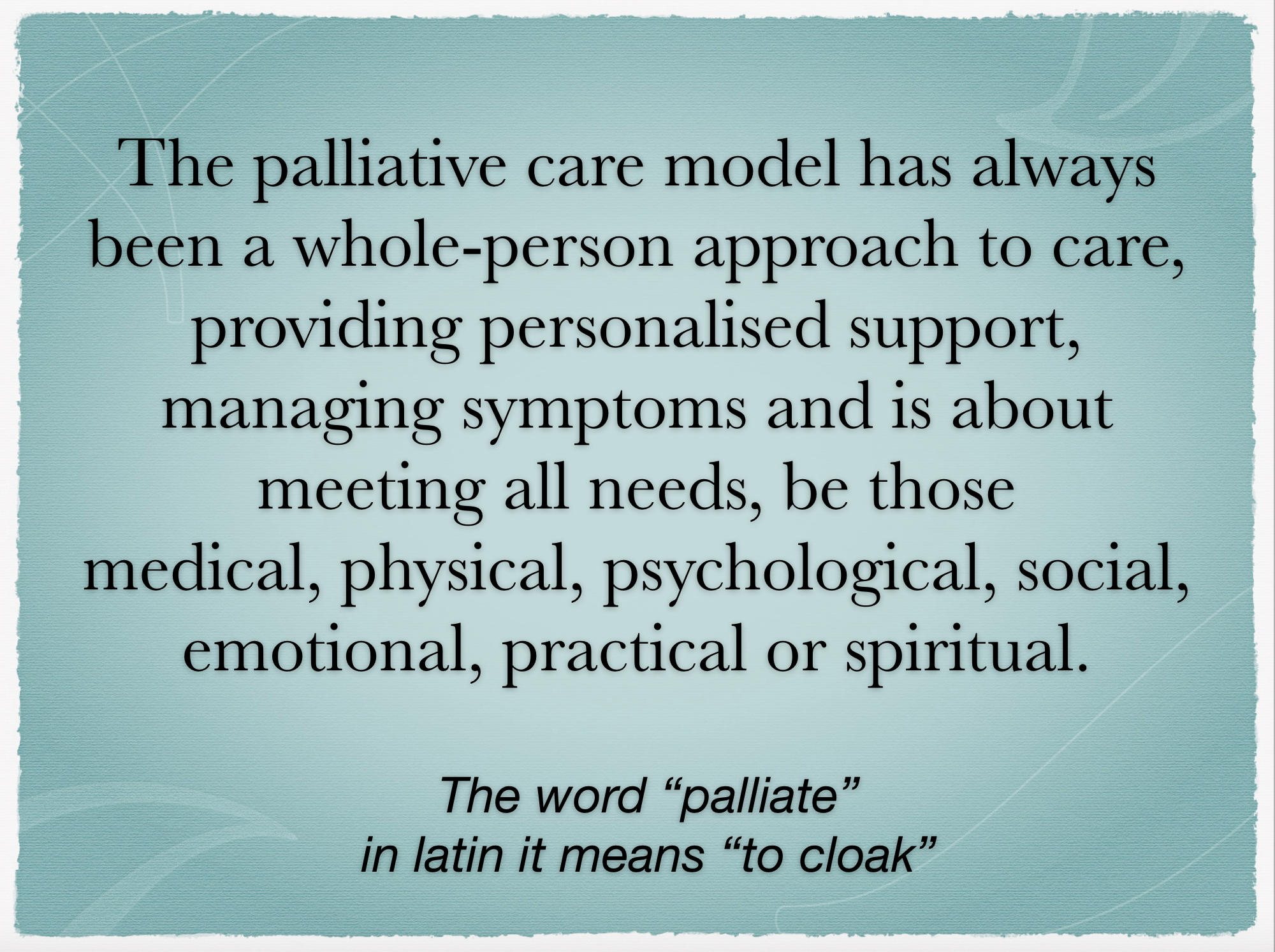
My early experience of healthcare was very paternalistic and not personalised at all, meaning it was not as good as it could’ve been. Fortunately, since then, I have built a fantastic team of professionals who embody personalised care and also my palliative care team whose care has always been personalised as the palliative model of care has always been about a whole-person approach, meeting all needs of the individual and supporting the person to live well.
The hospice and palliative care team have played a pivotal role in my life and in my care. It was my palliative care nurse, when doing my end of life planning, who became the first person to ever asked what mattered to me and what I wanted to do with my life now. No one had ever asked me that before. No one had ever taken the time to understand what I wanted for my life, what mattered to me and how they could facilitate that. The hospice and palliative care team have been instrumental in my care. They have helped fight for my care to be built around me, to have the care at home that I require and supported me to live well and be as active a patient as possible; they have enabled me and my family to self-manage my needs as much as possible.
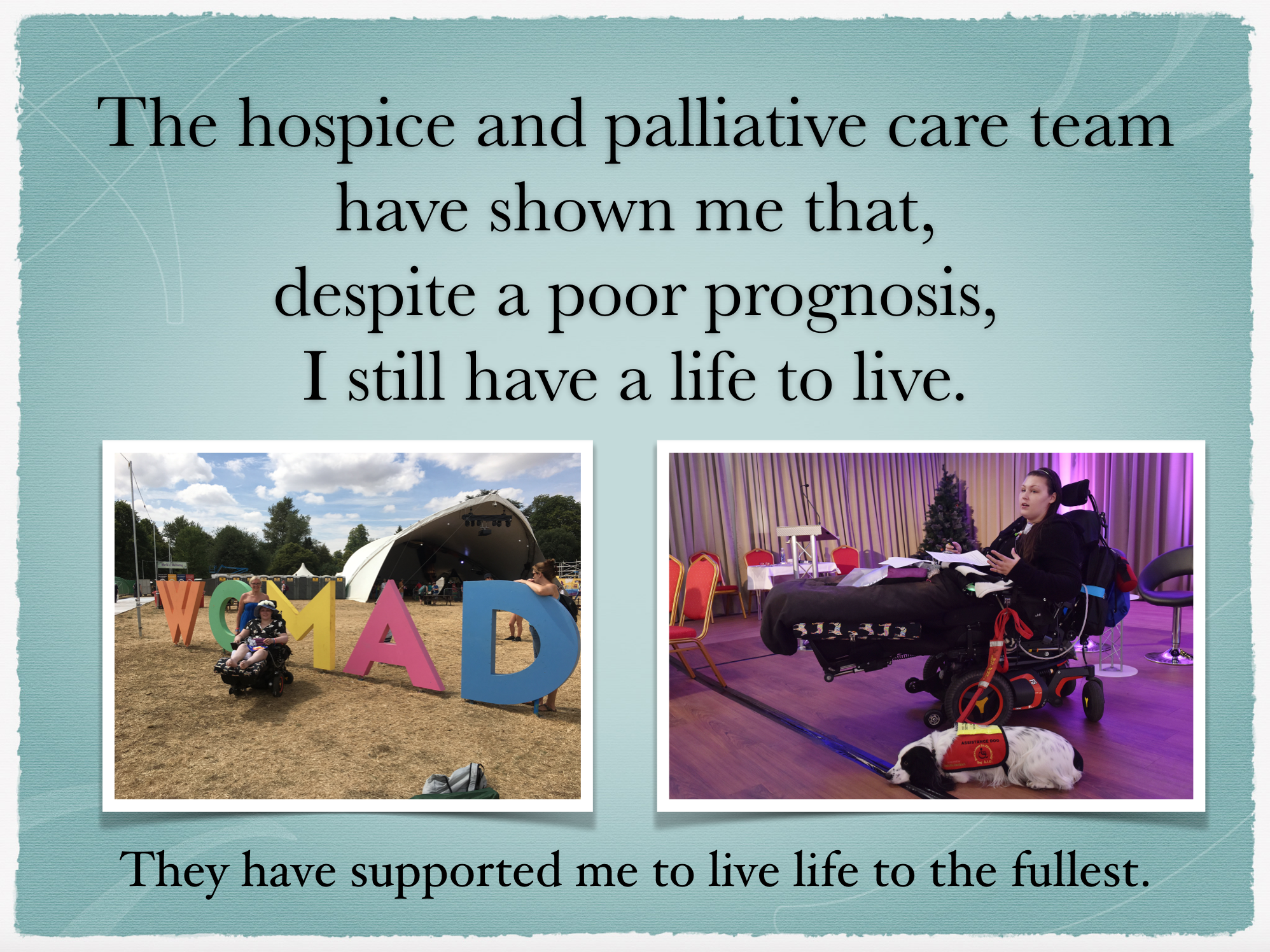
They showed us that despite a poor prognosis, I still have a life to live and have supported me to live life to the fullest. They have also worked hard alongside my NHS teams to best manage my symptoms and to facilitate the best possible quality of life for me.
The hospice also supported my NHS consultants in caring for me. I very much feel that initially, my NHS consultants felt like admitting I was going to die young was admitting defeat, that telling me there was no cure or even treatment, that they were somehow failing me. The hospice helped them to see that the absence of a cure did not cause the absence of good care; that they could provide me great care by focusing on me, my quality of life and what I wanted to achieve. Now my appointments are always about goals and outcomes, they always ask what I want out of an appointment to know how to support me and view and value me as part of my own medical team; something I believe is crucial in helping patients to become active in their own care.
At home, personalised care benefits me on a day to day basis. Over the years I have had social care direct payments, an integrated budget, Continuing Healthcare and a Personal Health Budget. I have my current care package, which I only received when my mum became ill in 2015 when she developed a brain tumour and then suffered a brain haemorrhage and then a stroke and developed epilepsy. After a battle, I secured this current package, which consists of 16 hours per day with an intensive care nurse, 8 hours overnight with a PA and 6 hours of double-up care during the day. Currently, the night care and double up care is provided via a Personal Health Budget and the nursing via an agency, but we will begin the process of moving the nursing onto the PHB soon.
Having always had control over my packages, always managing them ourselves with financial support from a broker, losing control of my package when mum became ill and I received a directly commissioned agency package, was tough mentally. I felt like my life wasn’t my own, I had my life dictated to me by people who didn’t know me and didn’t care to know me, and that what I wanted for my life was irrelevant. This had a damaging effect; I felt like I didn’t matter, what I wanted was unimportant and that no one truly cared about what I needed and wanted and how I felt. In fact, before securing this package and even since, I have been told by professionals that I am unreasonable to expect to stay at home due to how expensive my care is, and been told repeatedly I would be placed in a care home. I have won those battles, and I have the care I need, and am slowly regaining control over my life and care again.
Now, having some of my care on a PHB, I am partially in control of my care, and will be fully in control once the nursing is transitioned to the PHB. Then I will have total choice, control and autonomy over my life and care, which will be life-changing. It will mean my life is my own again, it is not dictated to me and I have the flexibility to make my care work for me.
My CCG likely wouldn’t admit it, but Personal Health Budgets are not their strongpoint. I have had to be the driving force and the expert in the process a lot of the time. Also, my CCG often purely view my Personal Health Budget from the lens of cost-saving, rather than a quality and outcomes perspective as I view it. Yes, it will save money – especially when you consider agencies can charge up to £15 or £20 per hour more than the cost of the staff’s wages, especially for nursing care – and cost savings and efficiency is important in order to meet the needs of the population in each area, I do not doubt how important cost saving is, but PHBs should not be viewed solely through this lens. It’s not just the direct cost savings, either, but my package has and will enable me to manage at home for longer, even in acute situations, saving money in the process; when you consider it would cost approximately £2500 per day to care for me in hospital, keeping me at home presents a huge cost saving. However for me, whilst cost saving is important, the ability to control my care, have choice over who cares for me, to have flexibility in my package to make it work for me and to have autonomy over my life and how I live it, are my priorities for the Personal Health Budget.
When I transitioned some of my care back to the PHB, I fought to have my mum provide most of the double-up care, which she provides 5 days a week with PAs doing the other 2 shifts. My CCG were reluctant, despite paying mum on a previous PHB, but I was able to evidence that this would achieve my outcomes best and also would prevent me seeking additional hours to facilitate any quality of life. My routine varies depending on events and outings, meaning the double-up care hours are rarely consistent and others providing the double-up care would mean fixing those hours and thus no ability to live my life and do my events. Mum, however, always comes to my events and is happy to do those 6 hours of double-up care to support me in what I want to do. I had to make a case to the CCG and that case was successful. This is one example of my CCG personalising my care and exercising their ability to adapt the frameworks to best meet the needs of the patient and their family. Yes, I had to fight for it, but my CCG have listened and agreed to this in order to best meet my desired outcomes.
Having the Personal Health Budget is what works best for me and meets my needs and outcomes in the most effective and efficient way. It must be appreciated a PHB is not right for everyone but also that, despite the right to have a PHB, many of my peers are prevented from accessing the life-changing benefits of a Personal Health Budget.
Personalised care requires a system-wide culture-change, the ability and willingness of individuals to be flexible and to adapt ways of working and to think outside the box. Often, as Jonathon’s story demonstrates, thinking outside the box can have tremendous benefits on various levels. Done well, personalised care transforms the lives of patients, and makes care more efficient and effective. I hope my story is just one example of personalised care done well and that it shows the direct benefit to patients and their families.
Thank you.



This Post Has 0 Comments