What if we viewed lived experience as an asset? As an asset of professional, economic,…

NHS Peer Leadership Academy: Day 1 of the First Residential
NHS Peer Leadership Academy Day 1
Well, what a day today has been. I write this late as we’ve been on the go all day. I am shattered. But it has been absolutely amazing. Meeting so many incredible people on this programme and making connections and friendships which will, I hope, last well beyond the three residential programmes as part of the Academy. It has been wonderful to meet people I know online face to face, and meet two young adults with life-limiting conditions, who are husband and wife, who are actually presenting in the same session at the Hospice UK conference.
How to reflect on today, when it was jam packed with so much greatness.
For starters, some of the participants met up last night at dinner so we’d already had some great conversations last night, and then whilst waiting for everyone to join us for the meeting.
We started off the day by introducing everyone and mapping out the programme, what it is and isn’t, where we’re heading and ensuring we’re all on the same page. Our first activity was talking on our tables about what we hoped the Academy would be, and what we hope it would not be – our “hopes and hope-nots”.

Rita then took us through how we got to where we are today with personalisation including personal health budgets, the different aspects of personalisation and where we as peer leaders fit in. We had some ‘estimation’ activities around the population, how many people over 65, over 80, and with long-term conditions. We discussed the changing demands on the NHS – which was founded to aid acute situations and provide acute care – and how now much of our demand on the NHS is for long-term conditions and ongoing needs, including a growing population of people with multiple conditions and complex health needs. People with long-term conditions are the larger consumer of health and social care services. We asked “Why here? Why now?” and the changing attitude shift and culture change that is improving the engagement and activation of patients in their own health, and in the health and social care sectors. We also talked about the financial aspect and the financial case for personalisation and about sustainability of the NHS and how we have to make a financial as well as personal case for personalisation and it is first and foremost about improving the lives of patients, but also using resources most efficiently, effectively and equitably.
This included a quote from Simon Stevens, Chief Executive of NHS England,
“We stand on the cusp of a revolution in the role that patients – and also communities – will play in their own health and care. Harnessing….this renewable energy is potentially the make-it or break-it difference between the NHS being sustainable or not.”
This was followed with a quote by James Sanderson, Director of Personalised Care at NHS England, which said:
“Empowering people to make choices and tailor their healthcare fundamental to the changes the NHS is seeking to make over the next few years. Ultimately, embedding these approaches at scale will encourage a shift in the relationship between the NHS and the people it supports. It is about moving towards a more equal relationship between services and people in all of our local communities.”
Colin then spoke about the different routes to how we all got to where we are today and we discussed on our tables how we got to where we are today.
Rita and Colin then went through the Comprehensive Model of Personalised Care, sharing the triangle that looks at where the different aspects of personalisation are aimed, for example social prescribing and shared decision making are universal for all, whereas in addition to these, people with long term physical and mental health conditions will also need personalised care and support planning and other services such as health coaching and self-management courses to help them manage their condition and its care and achieve maximum stability and benefit, and then specialist services which includes all of the above as well as integrated personal commissioning (IPC), personalised care and support planning through multidisciplinary teams as well as personal health budgets and integrated budgets.
After a break, we then had a discussion exploring personalised care amongst the whole group.
Jo then played a video of her son Mitchell who was one of the first people in the UK to have a personal health budget, sharing how his life was enhanced and his care managed efficiently, effectively and safely through his personal budget and the up-skilling of staff and building a team around Mitchell and his needs. We then had a chance to reflect on Mitchell’s journey and I shared some of my experiences of personal health budgets, agency care and so on.
Following a break for lunch, we came back to talk about personalisation, at its heart, being a shift in relationship. We looked at how and why it shifts, the fact that not all individuals have equal power, and about it’s not about giving all power to patients and carers, rather sharing power and collaborating to achieve the best outcomes. We discussed how the shift may be different on a personal level and a strategic level and where it all fits in and how and why it varies. We then, on our tables, were asked to share how we had experienced this shift, and I shared my experience of the fantastic care from my consultants who ask me what matters to me and what I want out of appointments, before sharing their desired outcomes, and then co-producing solutions. How they take an interest in my life and what’s going on and work hard to facilitate the life and quality of life I desire. Some on our table hadn’t had such a positive experience, and we noticed a clear disparity between the shift in care for people with physical/medical conditions, versus people with mental health needs. We talked about why this may be, and one conclusion was that it very much depends on the confidence and capability of the professional to open up dialogue, ask the patient what matters to them, ask the patient what they want to get out of an appointment/treatment/service and take the time to understand the patient – even if they then have to manage peoples’ expectations of what can be achieved in that appointment or within that service. So professionals’ confidence in having difficult conversations, willingness to ask and the capability to manage expectations and trying to achieve the best outcomes for that patient, and working in partnership with that patient.
After another break, we retuned for a session building on previous sessions and asking “How the shift in relationship informs the approach to co-production: facilitative leadership.” We discussed how to meaningfully engage individuals and about peoples’ different skills and how these can be best used. We discussed co-production in quite detail, especially strategic co-production, and how this requires a culture change. You can have all the policies, frameworks and strategies in the world but if the culture doesn’t adapt to allow these improvements and changes, then it will not succeed.
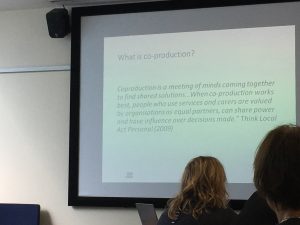
‘Co-production is a meeting of minds coming together to find shared solutions…. When co-production works best, people who use services and carers are valued by organisations as equal partners, can share power and have influence over decisions made’.
This led nicely onto our last activity on the day, were we completed the Myers-Briggs Personality Type assessment, trying to discover what type of personality we are and thus where our personality type, skills and unique perspective would be best used in the ongoing work on personalisation and personalised care. We didn’t do results today, so it was left that they would compile our individual results and we would come back to this tomorrow.
We then had a break for a few hours and we took Molly for a walk, before attending to some of my needs. We then met up for a drink in the bar before going to dinner, yet more opportunity to socialise.
I am really looking forward to tomorrow! I just hope I’ll sleep better tonight than I did last night – I only got 4 1/2 hours sleep last night because I couldn’t switch off for whatever reason.
Bring on tomorrow!
Molly dog has been such a good girl, our little star.







Great review – it looks like it was an intense day! Keep up your energy and enthusiasm!